Discover some of the staff of Western Australia’s longest serving hospital since the 1800s.
The work of Colonial Surgeon Dr John Ferguson, Radiologist William Hancock, Nurse Annie Kirkman, Dr Ethel Ambrose, Dr Harry Stephenson Lucraft, Dr Mercy Sadka, Nurse Robin Miller, Surgeon George Bedbrook, Professor Fiona Wood, Dr Robin Warren, Professor Barry Marshall, Professor Michael Lawrence-Brown and Radiographer David Hartley gives a glimpse into medical breakthroughs and changes in healthcare practices over the last two centuries.
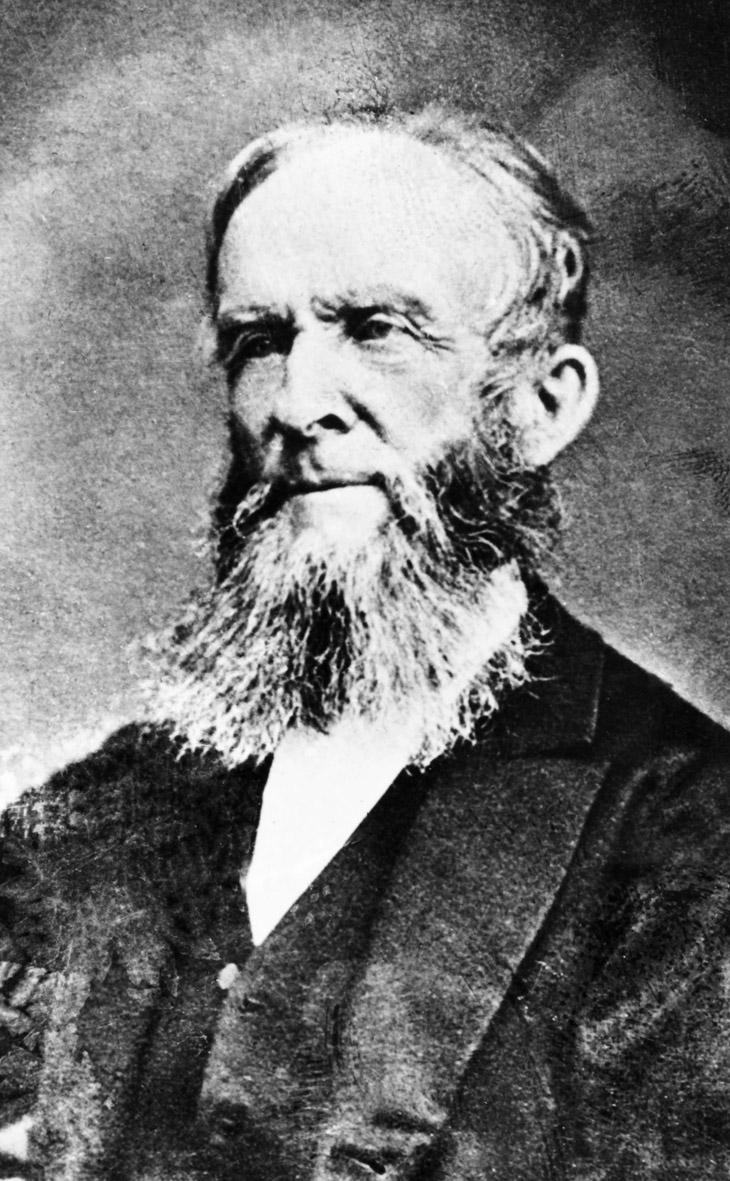
John Ferguson
c1802 – 1883
Colonial Surgeon
Physician and surgeon John Ferguson qualified in Edinburgh in 1822 and emigrated to Australia in 1842. He started farming in the Australind area, but his medical skills were soon in demand. When Colonial Surgeon, Joseph Harris retired in June 1846 Ferguson was offered the position.
At this time the hospital was run from a converted stable near the corner of St Georges Terrace and Barrack Street. Conditions were appalling. As the population and hospital admissions grew, Ferguson joined the community's call for a purpose-built Colonial Hospital and better health care.
The Colonial Hospital was opened in 1855 with Ferguson in sole charge until 1872.
Ferguson is believed to be the first in the Colony to use chloroform. He ordered the drug in April 1848, only six months after its initial test in England. In 1849 the Inquirer reported that Colonial Surgeon Ferguson had performed
“… a most satisfactory case of amputation, aided by the inhalation of chloroform … on a native patient whose leg was removed below the knee-joint without his exhibiting the least degree of consciousness.”
In 1852 Ferguson warned that the whooping cough epidemic could be particularly dangerous to Aboriginal people. He researched smallpox, promoted compulsory vaccination for children as early as 1860, and became a member of the Vaccination Board in 1861.
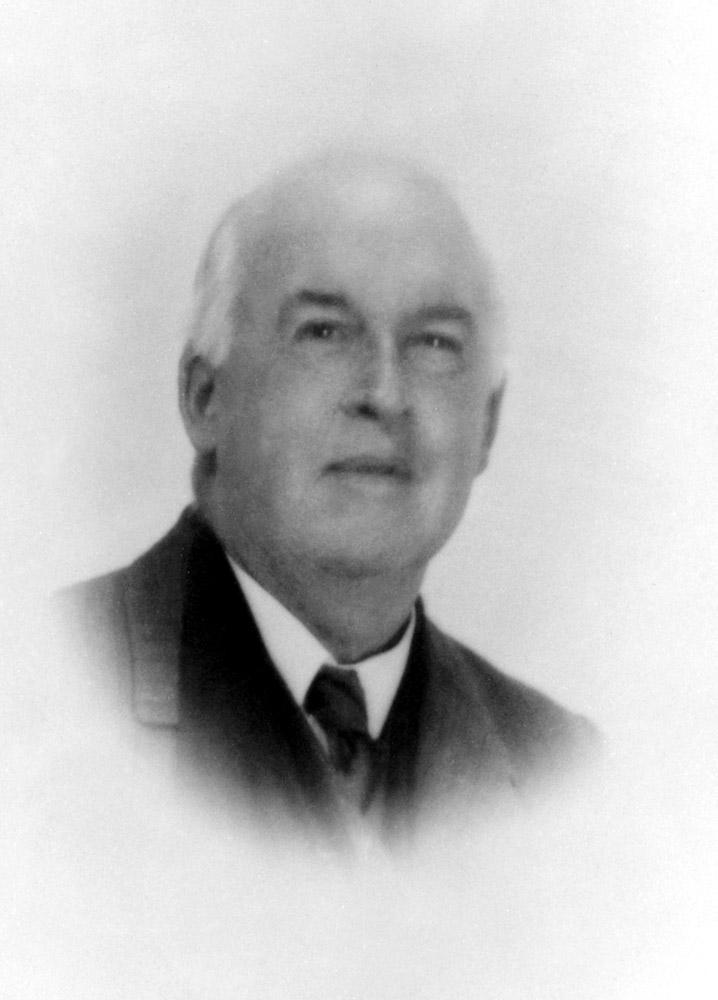
William Hancock
1863 - 1931
X-Ray Pioneer
One of the most valued artefacts in the Museum is a box of cold cathode X-ray tubes imported by the engineer, William Hancock, recognised as a pioneer in Radiology.
Born in Dublin, Hancock came to Perth in 1885 to take up the position of Superintendent of Telephones. His introduction to the Perth Public Hospital probably came through his later role as Government Electrical Engineer, where his advice regarding anything electrical was invaluable.
When X-ray was discovered in 1895, Hancock realised its huge significance and quickly obtained equipment from London. By 1896 he was able to produce X-rays in the newly named Perth Public Hospital.
His ground-breaking work was widely recognised both within and outside the hospital. In 1898 Hancock was appointed Honorary Radiographer at the hospital and the honorary degree of Doctor of Science was conferred on him in 1925 by the University of Western Australia.
When a central wing of the Hospital was built in 1904, two rooms were set aside for Hancock’s use and equipped to his design, including cupboards for storing glass plates.
Like many other pioneers in radiology, Hancock suffered from radiation sickness. He received injuries to his hands and eventually died in 1931 as a result of exposure to X-rays.

Annie Kirkman
1877 – 1965
Trained Nurse
On 19 December 1899, four nursing students received graduation certificates from the Perth Public Hospital. The first one was issued to Annie Kirkman and it is her name that has gone down in history.
When Kirkman’s career began only two substantial buildings stood on the Murray Street site – the 1855 Colonial Hospital and the 1894 Administration Building.
“I entered the Hospital on 1st January, 1896. It was not then a training school, as it was a very small hospital with only accommodation for 13 men and 9 women.”
Her accommodation was in the Colonial Hospital in bedrooms below street level. Conditions were harsh with long hours - from 7am until 9pm - with a 2 ½ hour break in the afternoon or evening, and just one day off a month.
“I think my most vivid and not-altogether-pleasant memory was the ringing of a very large and noisy bell at the early hour of 5.30am. This was sounded along the corridor, in each side of which were our bedrooms.”
In 1909, a four storey, purpose-built nurses’ home was completed which later became known as Kirkman House.
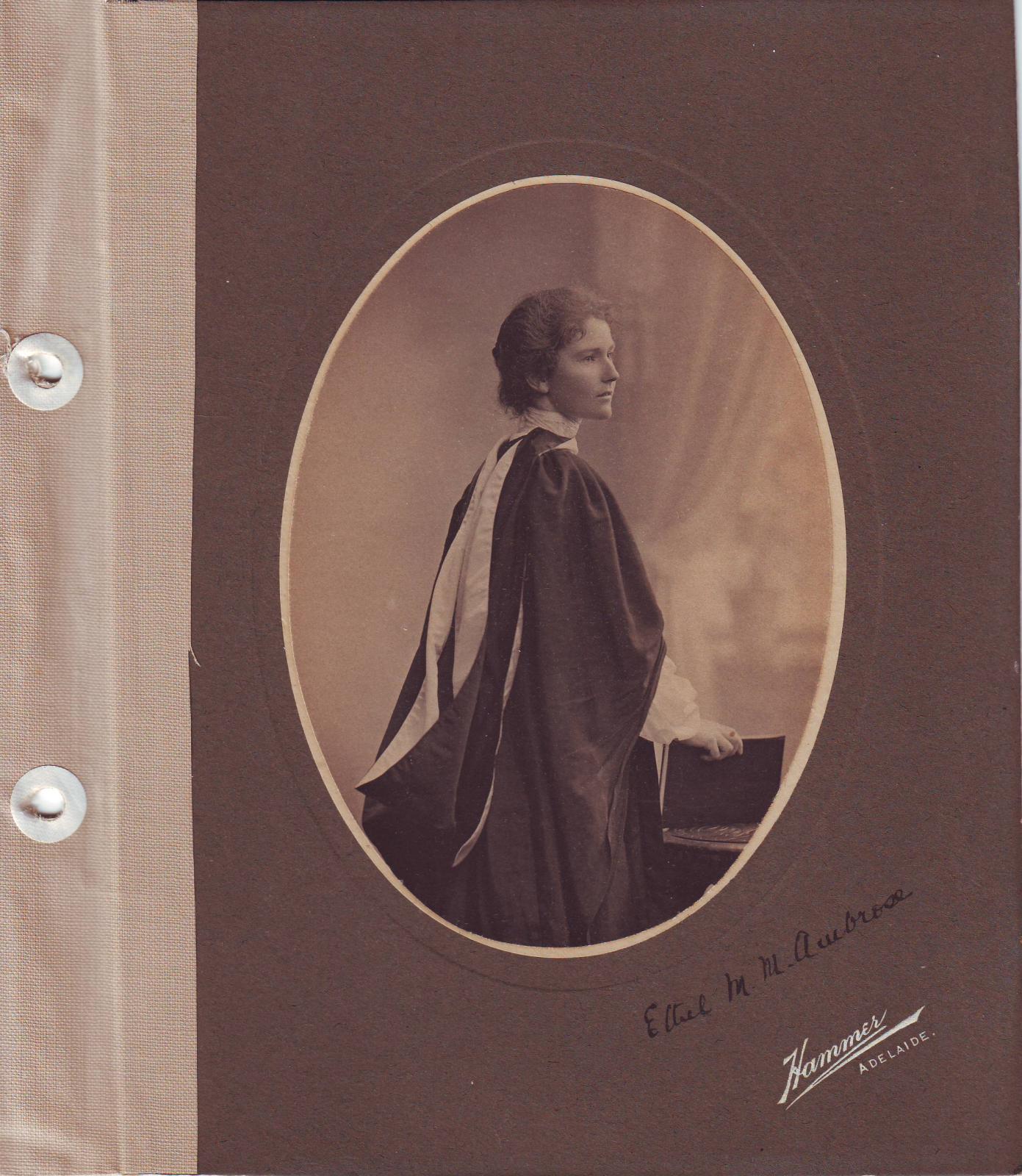
Ethel Ambrose
1874 - 1934
First Female House Surgeon
Dr Ethel Ambrose enrolled in medicine at the age of 23 and graduated from the University of Adelaide in 1903. On graduation, she came to Perth Hospital, as it was then known, to become the first woman doctor on the staff. Another member of the hospital, Dr Harvey Astles, was so appalled at her appointment that he sent in his resignation. He claimed,
"… it will be impossible to obtain from male patients the histories of past and present ailments”.
Astles’ complaints were disregarded and Dr Ambrose served at Perth Hospital for two years. However, her passion was to work as a medical missionary. She left the hospital in 1905 and joined her sister Lily, a nurse, at the mission hospital in Nasrapur, Poona, India.
Ambrose was concerned at the high infant mortality rate and, in 1909, moved to Pandharpur, a Hindu holy city. There she concentrated on medical care for women and children.

Harry S Lucraft
1894 – 1953
Physician & Photographer
Harry Lucraft was born in Adelaide and graduated in medicine at the University of Edinburgh. When World War I broke out he volunteered for active service. He was appointed Surgeon-Probationer on destroyers in the North Sea, during which time he developed an interest in photography.
In the 1920s, Dr Lucraft moved to Perth and entered a consultant practice in Lake Street with a special interest in cardiology and in 1928 he took up a position at the Perth Hospital as a Physician, where he worked until 1953. In this role, he improved the reputation of the Hospital through his clinical skill, teaching and patient care.
He was known as a skilled amateur photographer and was a member of the Van Raalte Club, a local photographic group whose members experimented to achieve soft effects and details in shadow.
The techniques had implications for radiology too, particularly because at that time X-rays did not capture detail. Using his skills in this area, Dr Lucraft did the clinical photography of the Hospital single-handed for many years. Eventually, he guided the development of a Department of Clinical Photography.
Harry Lucraft died in the Hospital he had served for twenty-five years.

Mercy Sadka AO
1923 – 2001
Ahead of her time
Marie Sadka, better known as Mercy, was influential in the early development of clinical neurosciences in Western Australia. After graduating from Oxford University in 1947, she became a Resident Medical Officer and Registrar at Royal Perth Hospital in 1948. Later she did post graduate training in neurology and neuropathology in the UK and US.
In 1959 Dr Sadka returned to RPH and was appointed Consultant Neurologist, where she worked for almost 30 years. During that time, she ran the Stroke Unit at Shenton Park Rehabilitation Hospital. Under her strong leadership the department became recognised as a model rehabilitation unit and enjoyed a high degree of stability over three decades.
The discovery of electroencephalography (EEG) in 1929 proved a ground-breaking diagnostic tool for neurological and psychiatric conditions. In 1959 Sadka introduced EEG into WA, first at RPH, and then at Princess Margaret and Sir Charles Gairdner Hospitals.
In 1988 she received the Order of Australia (AO) for services to the community.

Robin Miller
1940 – 1975
“Sugar Bird Lady”
Robin Miller graduated from nursing at RPH in 1963 and qualified as a pilot around the same time. She wanted a job that would combine both passions – nursing and flying. When she upgraded her private pilot's licence to a commercial one in 1966, nobody would employ a female pilot, no matter how qualified she was.
Her opportunity came when the second polio epidemic hit Western Australia in 1967. Although most people in the city had been vaccinated, many in regional WA had not. Miller bought a plane and boldly proposed to the Health Department that she fly the Sabin vaccination to people in the outback.
The oral vaccine was administered on a lump of sugar to disguise its bitter taste. Aboriginal children in regional Australia called her the ‘Sugar Bird Lady’. Miller administered over 37000 doses of the vaccine. She was later offered a position with the Royal Flying Doctor Service.
“A strange job for a girl many people say when referring to my particular work. To me it’s normal. I was brought up with aeroplanes, (my father is a pilot) and I have always been keenly interested in medicine – stimulated by my training at RPH!”
Robin Miller died of cancer in 1975 at the age of 35.

George Bedbrook OBE
1921 – 1991
Paralympics Pioneer
George Bedbrook was the Director of the Paraplegic Unit at RPH Shenton Park Annex from 1954 to 1972 where he pioneered the use of sport and exercise in rehabilitating people with spinal injuries.
Sir Ludwig Guttman, who founded the Stoke Mandeville Games (the forerunner to the Paralympics), visited RPH in 1956. Guttman inspired Bedbrook to bring organised sport for people with disabilities to Australia. Bedbrook established hospital sport days which gave the rehabilitation a competitive focus. As he said:
“Competitive and team sports provide a physical and psychological stimulus far more profitable than routine remedial exercises. Not only do these activities develop and strengthen the body musculature and promote coordinated movements, but also of equal importance they recreate the sense of comradeship and normal human association...”
Bedbrook led Australia’s first team for athletes with a disability to the 1957 Stoke Mandeville Games in England. Three years later, he facilitated the attendance of the Australian Paralympic Team at the first Paralympic Games in Rome, Italy. Two years later, in 1962, he was the primary organiser when Perth hosted the first Commonwealth Paraplegic Games.
Sir George Bedbrook was knighted in 1978 for his contribution to the care of people with paraplegia.

Fiona Wood AM
1958 –
Inventor of Spray-on Skin
Professor Fiona Wood is one of Australia’s most respected plastic and reconstructive surgeons and a leading burns specialist. In 1991 Wood qualified as Western Australia’s first female plastic surgeon and went on to become the Director of the Burns Unit at Royal Perth Hospital.
She began working with medical scientist Marie Stoner in 1993 on a method for burns treatment. From this collaboration an entirely new, and more successful, method of treatment was developed. It was a technique of spraying new skin cells on to burns to close wounds as quickly as possible. A small shaving of skin is taken from the patient, placed in a formula, then sprayed onto the patient using an atomiser. There it reproduces the skin cells on the body.
The spray-on skin was first used in 2002 following the Bali bombings. Twenty-eight survivors of the terrorist attack were flown to RPH. Wood led a team and saved 25 patients who were suffering from severe burns, deadly infections and shock. This major operation involved four operating theatres, 19 surgeons and 130 medical staff working around the clock.
Professor Wood was named a Member of the Order of Australia (AM) in 2003 and in 2005 she was named Australian of the Year.
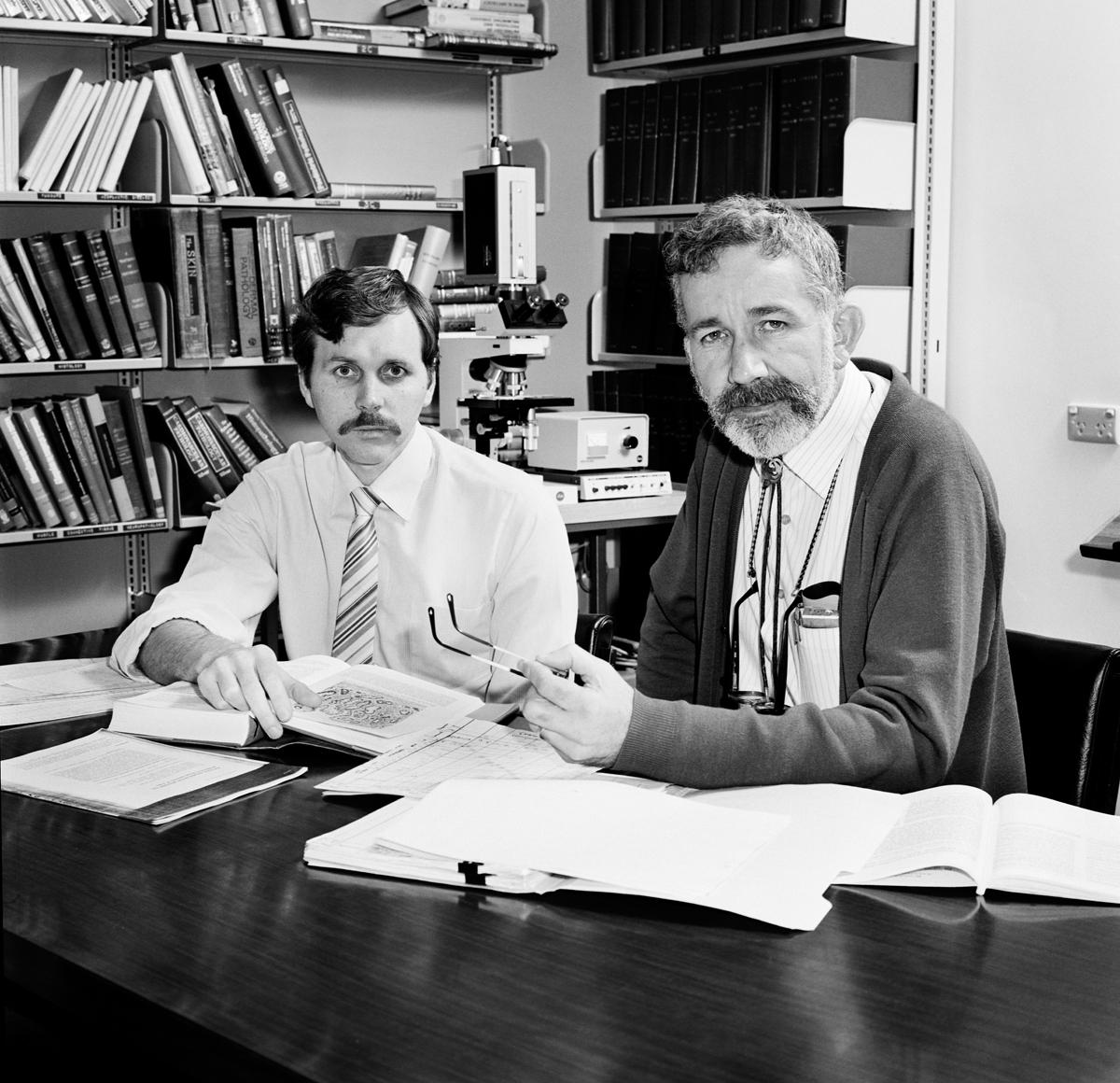
Robin Warren & Barry Marshall
1937 - 1951 -
Nobel Laureates
Dr Robin Warren arrived in Perth in 1968 to take up the position of pathologist at RPH. In 1979, he detected bacteria growing on the surface of a gastric biopsy. He collected samples and showed firstly that they were usually related to chronic gastritis, and secondly that they were not found normally in the stomach. This began a research program that led to an astounding breakthrough in medicine.
In 1981, he was joined by Barry Marshall, who had moved to RPH in order to further his training as a specialist physician. As part of his training Marshall began working with Dr Warren and they decided to undertake a more thorough study. They discovered a previously unknown bacteria, helicobacter pylori, to be the actual cause of gastric ulcers.
At one stage, when they had difficulty in getting the results of their research recognised, Marshall infected himself with the bacteria. He became very ill, but when he treated himself with antibiotics the infection was cured. This discovery revolutionised the diagnosis and treatment of peptic ulcer disease.
In 2005 Professor Barry Marshall and Dr Robin Warren were awarded a joint Nobel Laureate in Physiology or Medicine for their ground-breaking research.

Michael Lawrence-Brown & David Hartley
1944 - 1938 -
Inventors & Innovators
Prominent RPH vascular surgeon Michael Lawrence-Brown and radiographer David Hartley worked together in search of a less-invasive way of treating diseases of the arteries than open surgery.
In 1994 they created the prototype for one of the world’s first intra-aortic stents, known as the Endostent. The Dacron tube-shaped device with stainless steel springs is inserted in the ruptured aorta – the largest artery in the body - to hold it open so blood can continue to pass through.
Professor Lawrence-Brown and Mr Hartley’s innovative invention was aided by a model they named ‘Mr Walker’. They devised introducing systems and practiced their technique on Mr Walker when a spare X-Ray fluoroscopy table was available.
The first prototype stent-grafts were hand stitched by Hartley at his office desk until the Hospital found a dedicated space in Kirkman House. Here they were joined by Sister Sue Morriss from the Vascular Surgery Theatre. She introduced principles of Clean Room production and expertly stitched and assembled the rapidly increasing number of devices required for Clinical cases. As the project developed and more staff were needed, the Endostent project moved into a unit in the Medical Research Foundation.